what causes red man syndrome
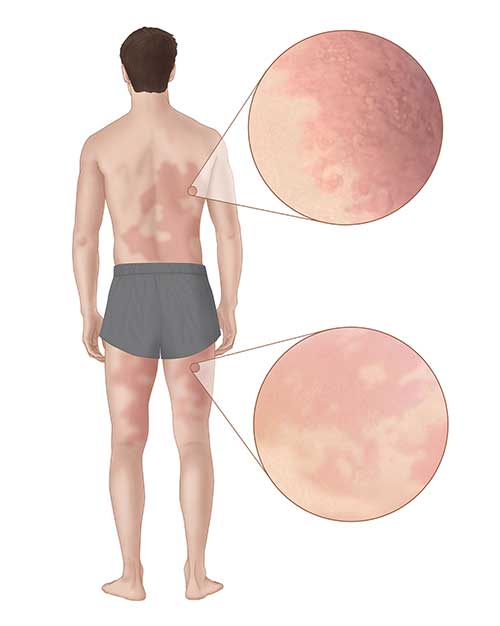
 Red Man Syndrome: Symptoms, Treatment, Picture, and More
Red Man Syndrome: Symptoms, Treatment, Picture, and MoreWarning: The NCBI website requires JavaScript to operate. NCBI Bookshelf. Service of the National Library of Medicine, National Institutes of Health. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan... StatPearls [Internet]. Red Men Syndrome Thomas J. Martel; Radia T. Jamil; Kevin C. King.AuthorsAfiliations Last Updated: January 20, 2021. Continuous educational activity Red man syndrome (RMS) is an anaphylactoid reaction caused by the rapid infusion of antibiotic glcopeptide vancomycin. RMS consists of a pruritic eruption, erythematous of the face, neck and upper torso, which can also involve the extremities, although to a lesser degree. Symptoms may include weakness, angioedema and chest or back pain. RMS is caused by vancomycin through the direct and non-mediated release of the histamine of chewing and basophile cells. The amount of histamine release is usually related to the infused dose of vancomycin and the infusion rate. RMS is usually associated with faster infusion rates, but can be seen after slower infusion rates and after several days of transfusion. Practitioners who use vancomycin must be aware of this drug reaction, its prevention and treatment. This activity describes the evaluation, diagnosis and management of red man syndrome and highlights the role of team-based interprofessional care for affected patients. Objectives:Introduction Red man syndrome (RBC) is an anaphylactoid reaction caused by the rapid infusion of antibiotic glcopeptide vancomycin. RMS consists of a pruritic eruption, erythematous in the face, neck and upper torso, which can also involve the limbs to a lesser degree. Symptoms may include weakness, angioedema and chest or back pain. RMS is caused by vancomycin through the direct and non-mediated release of the histamine of chewing and basophile cells. The amount of histamine release is usually related to the infused dose of vancomycin and the infusion rate. RMS is usually associated with faster infusion rates, but can be seen after slower infusion rates and after several days of transfusion. Practitioners who use vancomycin must be aware of this reaction, its prevention and treatment. EtiologyRMS occurs more often with intravenous vancomycin, but may rarely occur from oral or intraperitoneal vancomycin. It is often related to a rapid infusion rate of vancomycin (1 gram in less than 1 hour). Current treatment recommendations are to administer vancomycin at a rate not faster than 1 gram/hour or 10 mg/min. RMS often starts from 4 to 10 minutes from the start of the first dose of intravenous vancomycin. It can occur later during infusion or start soon after the end of the dose. RMS can occur from later doses to seven days. The increase in the incidence of methicillin/oxacillin resistant to stafilococcus aureus, polyresistent Staphylococcus epidermidis, resistant to penicillin Streptococcus pneumoniae, and the Clostridium difficile resistant to metronidazol has resulted in an increase in the use of vancomycin. Vancomycin is commonly used to treat bacterial endocarditis, cellulite abscesses, postoperative wound infections, surgically placed infected devices and central bloodstream infections associated with the line. There are cases of RMS that occur from other antibiotics such as rifampin, cefepime, teicoplanin, ciprofloxacin and amphotericin B.EpidemiologyRMS is the most common adverse reaction to intravenous vancomycin. It is presented in 4% to 50% of infected patients treated with intravenous vancomycin. Patients under the age of 40 are at increased risk of severe RMS reactions. Serious reactions include angioedema, hypotension, tachycardia, weakness, muscle spasms and chest or back pain, as well as an eruption of the face, neck and upper torso. RMS is usually smooth and easy to handle. There are rare cases of life threatening RMS reactions. PatophysiologyVancomycin was discovered in 1952 on soil obtained from the forests of Borneo. The initial preparations for the antibiotic lacked purification and were brown. Therefore, many referred to vancomycin as "Lodo Mississippi". Clinicians initially thought that RMS, otic and renal toxicity were secondary to impurities in vancomycin. However, even after the purification of vancomycin, the security services management system continued to be observed. Animal and human studies indicate that vancomycin activates the degranulation of mast and basophile cells by increasing the release of histamine. The amount of histamine release has been correlated with the dose and rate of vancomycin infusion. However, not all studies correlate high levels of histamine with severe cases of RMS and suggest that histamine metabolism can also be delayed due to inhibition of the enzymes of N-methyltransferase histamine and oxidase diarrhea. History and Physics The clinical presentation of RMS can vary, from minor pruritus to occasionally symptoms that threaten life. Symptoms can occur as soon as four minutes after starting the first dose up to seven days after the end of the dose. Patients with infections treated with intravenous vancomycin are at risk of developing RMS. Signs and symptoms of RMS include: Evaluation The diagnosis of RMS is performed clinically and does not depend on laboratory tests or other tests. Serious cases should be differentiated from anaphylactic reactions mediated by IgE. Treatment / Management When a patient develops RMS, intravenous antibiotic infusion should be stopped immediately. Support attention should be provided. H1 (diphenhydrmine) and H2 antihistamines (ranitidina or cimetidine) are used in the management of RMS. In most cases, future doses of vancomycin may be given at lower infusion rates. Mild cases (smooth and mild pruritus) can be given with antihistamines such as diphenhydrmine 50 mg by mouth or intravenous and ranitidine 50 mg by IV. Most episodes will resolve within 20 minutes, and vancomycin can be restarted to 50% of the original rate. Future doses should be given at the new slower rate, usually more than two hours. Cases moderate to severe (see rash, hypotension, tachycardia, chest pain, back pain, muscle spasms, weakness, angioedema) must be handled according to gravity. Patients with severe symptoms should be evaluated for anaphylaxis or other serious cause of their symptoms before assuming red man syndrome. If, after a careful evaluation, the patient is determined to have RMS, antihistamines such as diphenhydramine and ranitidine may begin intravenously. Normal saline intravenous bowls are used to treat hypotension. After the symptoms are resolved, vancomycin can restart and manage more than four hours. If there are antibiotics alternative to vancomycin, they should be used. If vancomycin should continue, patients should be pre-medicated with diphenhydramine 50 mg intravenously and ranitidine 50 mg intravenously 1 hour before each dose, and vancomycin should be given for four hours under close observation. If the symptoms of anaphylaxia are present, such as mental condition disorder, hypotension, stridor, shortness of breath, wheezing and urticaria, treatment should begin immediately for anaphylaxia, and the patient needs emergency care. Epinefrine should be given early, and the patient may have an epinefonic auto-injector with them, which can be used. Emergency medical services, if available, should be activated immediately to accelerate the treatment and transport of patients to definitive care. Patients who require rapid infusion of vancomycin may be treated with diphenhydramine and ranitidine. However, the best preventive measure to prevent SCR is to keep infusion rates below 10 mg/min. Differential Diagnosis Diagnosis should be differentiated from an anaphatic reaction. Both RMS and anaphylactic reactions will have similar findings of pruritus, erythematous and tachycardia. Anaphylactic reactions involve stridor, angioedema, hives and bronchoespasm wheezing. Anaphylactic reactions are mediated by IgE and require prior exposure. RMS is an adverse anaphyloid reaction related to the rate that occurs most often during the first exposure to intravenous vancomycin. Prognosis The prognosis for patients with RMS is excellent with proper management. Vancomycin can be used again after an episode of RMS. Appropriate precautions and treatment guidelines should be followed. Normal intravenous saline should be used to treat hypotension, and other supportive care measures should be provided. Complications Red man syndrome is caused by the release of histamine from basophiles and the masculine cells by antibiotics such as vancomycin. Symptoms include a red rash, hypotension, tachycardia, angioedema, etc. Although most cases are manageable, some may be life-threatening. Deterrence and Patient EducationMedical care providers must be aware of the presentation of red man syndrome, as well as the management of this condition to improve patient outcomes. Patients should receive the most appropriate care and be educated on condition. Pearls and Other Issues Key Points Key Points Improvement of Health Team Results To help maximize patient care and patient safety, it is important for the health care team to:Continue education/review QuestionsReferences This book is distributed under the terms of the Creative Commons 4.0 International License ( Creative Commons 4.0), which allows the use, duplication, adaptation, distribution and reproduction in any medium or format, provided that you give appropriate credit to the original author(s) and source, a link to the Creative Commons license is provided, and changes are indicated. ViewsIn this PageRelated information Similar products in PubMed Recent activityYour navigation activity is empty. The activity recording is off. , 8600 Rockville Pike, Bethesda MD, 20894 USA

Red Man Syndrome: Symptoms, Treatment, Picture, and More

Red man syndrome causes, symptoms, diagnosis, treatment & prognosis

Red Man Syndrome: Causes, Symptoms and Treatments | Nursing school survival, Nursing school studying, Critical care nursing

Red Man Syndrome Causes, Treatment, and Symptoms - YeyeLife

Red Man Syndrome|Causes|Signs|Symptoms|Treatment|Prevention

Red Man Syndrome: Symptoms, Treatment, Picture, and More

PDF) Skin Color Induced by Food and Drugs-Red Man Syndrome-1.vancomycin

Red Skin Syndrome: Stages, Treatment, Healing, and More

Red man syndrome: Symptoms, treatment, and pictures

Pin on Nurse stuff
Erythroderma | DermNet NZ

Health Red man syndrome disease - www.24wikiss.blogspot.com

Antibiotics: Part II. - ppt video online download

Adverse drug reaction - Wikipedia
PDF) Vancomycin-induced red man syndrome in pediatric oncology: Still an issue?

Red man syndrome: Symptoms, treatment, and pictures

Red Man Syndrome- Causes, Treatment and Management
RED MAN SYNDROME CAUSES - Vancomycin induced Red Man Syndrome | Semantic Scholar

Red Man Syndrome: Symptoms, Treatment, Picture, and More

Emergency Dermatology Dr Melissa Barkham Spotlight Seminar 30 th September ppt download

Red Man Syndrome | Med Health Daily

Shoulder Arthritis / Rotator Cuff Tears: causes of shoulder pain: Red man syndrome

Redman Syndrome Pictures

Erythroderma | DermNet NZ

Erythroderma | DermNet NZ

Red Man Syndrome Adverse Reaction following Intravenous Infusion of Cefepime | Antimicrobial Agents and Chemotherapy
Cutaneous adverse reactions to antibiotics | DermNet NZ

Red Skin Syndrome - Eczema Association of Australasia Inc

What Is the Connection between Vancomycin and Redman Syndrome?

Perioperative anaphylaxis: pathophysiology, clinical presentation and management - BJA Education
Do Cis Men Have Periods? The Truth About Irritable Male Syndrome
Drug-Induced Hypersensitivity Reactions: Cutaneous Eruptions

Red Skin Syndrome - Eczema Association of Australasia Inc

Red-man syndrome after vancomycin: potential cross-reactivity with teicoplanin | Postgraduate Medical Journal

Red-man syndrome after vancomycin: potential cross-reactivity with teicoplanin | Postgraduate Medical Journal
Alpha-gal Allergy | Ticks | CDC

Vancomycin - Wikipedia

Shoulder Arthritis / Rotator Cuff Tears: causes of shoulder pain: Red man syndrome

RED MAN SYNDROME CAUSES - Vancomycin induced Red Man Syndrome | Semantic Scholar

Brief communication: MRGPRX2, atopic dermatitis and red man syndrome. - Abstract - Europe PMC
Posting Komentar untuk "what causes red man syndrome"